The course of pregnancy is influenced by many factors. High risks carry the Rhesus conflict of the mother and fetus. However, not everyone understands the causes of this phenomenon, which causes fear of the unknown. Therefore, every expectant mother is obliged to know what the Rh factor is dangerous and in what cases the Rh-mother-fetus conflict occurs.
Rhesus conflict - what is it?
To understand the essence of the problem, it is important first of all to understand the importance of the Rh factor. It is a special protein located on the surface of red blood cells. This protein is present in the blood of 85% of all people, and the rest is absent. Therefore, the first of them are considered owners of a positive Rh factor, and the second negative.
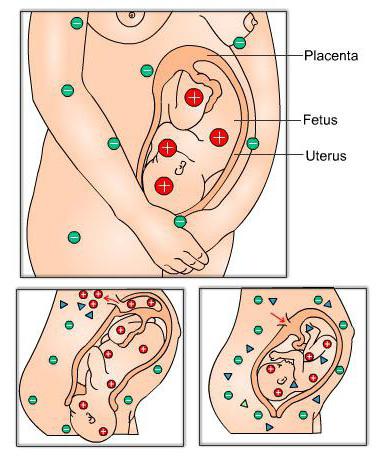
Thus, it determines the immunological characteristics of the body and does not affect human health at all. The Rh factor is usually denoted by Rh + and Rh-. This term was first introduced in 1940 by scientists Alexander Wiener and Karl Landsteiner. The Rh conflict of the mother and the fetus is an immunological incompatibility with the Rh factor of the blood if the mother is negative and the fetus is positive. The danger of the Rhesus conflict is that it can cause fetal death of the fetus, stillbirth, miscarriage. This phenomenon can appear in a future mother with a negative Rh both in the process of bearing the fetus and during childbirth. An immune conflict between the mother and the fetus occurs if the fetus inherits Rh + from the father.
Causes of the Rhesus conflict of mother and fetus
For the body of a future mother, the blood of a baby with Rh + is a serious threat, therefore, it produces antibodies that respond to the fetal red blood cells and destroy them. The rhesus conflict of the mother and the fetus is explained by the transplantation of the red blood cells of the fetus with a positive Rhesus factor into the mother’s blood with a negative indicator.
The immunological conflict is largely due to the outcome of the first pregnancy of a woman. During gestation, the Rh conflict may be due to blood transfusions, in which the Rh factor was not taken into account, previous abortions, miscarriages. Also, the Rh incompatible blood of a child can enter the bloodstream of the mother during obstetric care, so the mother's body becomes susceptible to a negative Rh factor, and the likelihood of a Rhesus conflict during the second pregnancy increases. The risk of isoimmunization increases with caesarean section. Blood incompatibility can be triggered by bleeding during pregnancy and childbirth as a result of damage to the placenta.
The likelihood of Rhesus conflict by blood type
The Rh factor is a genetically determined and dominant inherited trait. If the mother has negative Rh and the father positive with homozygosity, the child always receives Rh +. In this case, the risk of blood type conflict is very high. And in the case of the father’s heterozygosity, the probability of transmitting to the fetus a negative or positive Rh is equal.
At the eighth week of fetal development , hematopoiesis occurs, during which red blood cells are more likely to enter the bloodstream of the mother. In this case, the protection of the mother’s immune system is triggered, since the antigen of the fetus is considered foreign. Therefore, the pregnant woman’s body produces anti-Rhesus antibodies, which causes the Rh conflict of the mother and fetus. The risk of immunological conflict during gestation is quite small and amounts to only 0.8%, but it is very dangerous, therefore, it requires special study and attention. To identify approximately Rh of the unborn child according to the analysis of the blood type of the parents, forecasting for the Rh conflict during pregnancy will allow. The table illustrates the likelihood of blood incompatibility.
Consequences and threats during Rh conflict during pregnancy
An immune conflict between mother and fetus is fraught with serious consequences for the child. Antigens produced by the mother’s body, having discovered a foreign body with an incompatible Rh factor, penetrate the fetal blood stream through the hematoplacental barrier and destroy the baby’s blood formation, inhibiting the formation of red blood cells.
This behavior of antibodies can cause an extremely dangerous condition for the fetus, threatening the life of the unborn child, which is characterized by acidosis, hypoxia, anemia. An excessive amount of fluid accumulates in the baby’s body and development of almost all systems and organs is impaired. In the event that measures are not taken in a timely manner, there is a serious threat of miscarriage, fetal death, stillbirth, the birth of a child with a hemolytic disease, which will continue to progress due to the accumulation in the baby’s body of anti-Rhesus antibodies, the development of which caused a conflict between the mother and the fetus during pregnancy . It can also cause developmental pathologies, which are expressed in an excessive increase in the internal organs, brain, heart, and toxic damage to the central nervous system.
Symptoms
Rhesus conflict of mother and fetus during pregnancy does not have clinical manifestations and specific symptoms. It is possible to identify the problem only by conducting a laboratory blood test, which shows the presence of antibodies to a negative Rh factor.
In a fetus, blood incompatibility is manifested in the development of a hemolytic disease of the internal organs and body systems, which can lead to its death during the period from 20-30 weeks of pregnancy, as well as to miscarriage, stillbirth, and premature birth.
In addition, an edematous, icteric, and anemic form of hemolytic pathology may appear in a full-term baby. Rhesus conflict in the fetus is manifested in the appearance in the blood of immature red blood cells, pathologies of the development of internal organs. Symptoms are determined by the amount of antibody produced by the mother's body. In severe form, the disease occurs when the swelling of the fetus occurs - an increase in the size of internal organs, the appearance of ascites, an increase in the placenta and amniotic fluid volume are observed. The mass of the child can be increased up to two times, the disease is often accompanied by dropsy.
Laboratory research
Rhesus-conflict "mother-fetus" during pregnancy can prevent early diagnosis, primarily in the form of identifying Rhesus factors of the father and mother before the onset of future pregnancy or in its early stages.
Prediction of the Rh conflict is based on data on previous blood transfusions, the course and outcome of the first pregnancy, the presence of abortions, miscarriages, fetal death inside the mother’s womb, and hemolytic illness of the child, which makes it possible to reliably identify the risk of isoimmunization.
Laboratory blood tests for the determination of anti-Rhesus bodies and titer are performed for all women with suspected Rh conflict during pregnancy. Analyzes should be taken and the father of the child. If the likelihood of a Rhesus conflict is high, a pregnant woman needs to be tested every month. From the 32nd week, laboratory tests are carried out twice a month, and from the 36th week - every week until delivery. If a Rhesus conflict is detected during pregnancy, studies will determine the content of antibodies in the mother's body. The earlier the pathology is diagnosed, the lower the risk of complications, since the effect of the Rh conflict accumulates over time.
Ultrasound and invasive methods for assessing risk to the fetus
In order to diagnose in more detail the immunological conflict of the fetus and the mother, an ultrasound scan is performed at least four times from the 20th to 36th week of pregnancy, as well as before delivery. Ultrasound allows you to track the features of the development of the fetus, as well as to identify the presence of pathologies.
In the process of the study, the state and size of the placenta, the volume of the abdomen of the fetus, amniotic fluid, dilated umbilical veins are evaluated.
Additional research methods are ECG, cardiotocography, phonocardiography, which allow the fetus to determine the level of hypoxia in the Rh conflict. Valuable information is provided by invasive assessment methods - the study of amniotic fluid by amniocentesis and umbilical cord blood through cordocentesis. Diagnosis of amniotic fluid allows you to determine the titer of anti-Rhesus bodies, the sex of the child, the maturity of the fetal lungs. The exact degree of the pathology is diagnosed by cardiocentosis according to the blood group and the Rh factor of the fetus in umbilical cord blood. In addition, studies show the presence of whey protein, the content of hemoglobin, bilirubin, reticulocytes, antibodies, fixed on red blood cells.
Treatment
If there is a conflict between the mother and the fetus over the blood group, the only effective way of treatment is to transfuse the fetus through the umbilical cord vein inside the womb. The procedure is carried out under the control of ultrasound. This measure allows you to alleviate the condition of the fetus, extend the gestation period, reduce the manifestations of anemia, hypoxia.
To weaken the influence of the Rhesus conflict, oxygen therapy is also carried out, a course of non-specific therapy is prescribed, which includes vitamins, preparations containing iron, calcium, antihistamines. If the fetus has a serious condition, then a cesarean section is performed at 37-38 weeks of pregnancy. Also, a pregnant woman is prescribed plasmapheresis, which allows to reduce the content of antibodies in the blood to the red blood cells of the fetus.
After birth, the child undergoes a replacement blood transfusion to replace decaying red blood cells and is prescribed treatment for hemolytic pathology - droppers that remove toxic substances from the body and reduce the level of red blood cell decay, irradiation with ultraviolet rays. Treatment requires an enhanced course of therapy, monitoring by neonatologists, sometimes the child is placed in the intensive care unit. Breastfeeding is not recommended during the first 2 weeks after birth if a hemolytic disease is detected.
Childbirth in Rh conflict
Most often, the outcome of pregnancy in the presence of a Rhesus conflict is a premature birth. Therefore, the task of doctors is to extend the period of bearing a child, comprehensive monitoring of the process of its development. For diagnosis throughout the duration of pregnancy, an ultrasound scan, dopplerometry, CTG are performed. If further bearing is a serious danger to the fetus, a decision is made on childbirth ahead of schedule.
In most cases, the bearing of the fetus during a Rhesus conflict ends with a cesarean section. Childbirth naturally occurs extremely rarely and only if the condition of the fetus is assessed as satisfactory and the baby is not in danger. Caesarean section is considered the most safe and gentle for the fetus. During childbirth, the presence of a neonatologist is necessary for resuscitation if necessary. Obstetrics should be carried out in a well-equipped room with all the necessary medical equipment and under the supervision of highly qualified doctors.
Preventative measures
The mother-fetus conflict during pregnancy can cause serious consequences for the baby. Therefore, preventive measures aimed at preventing Rh conflict and the development of isoimmunization are of great importance. When blood transfusion, it is important to consider compatibility with the donor, it is necessary to maintain the first pregnancy, as well as to prevent abortion. Careful planning of pregnancy is of no small importance. The study of blood type, Rh factor will prevent Rhesus conflict during pregnancy. A blood group compatibility chart avoids future problems. Care should be taken in the course of pregnancy. As a prophylaxis, an intramuscular injection of an anti-Rhesus immunoglobulin from a blood donor to women with a negative Rh factor and with increased susceptibility to a positive antigen is used. This drug destroys red blood cells that have fallen from the carrier of a positive Rh factor, thereby reducing isoimmunization and the risk of Rh conflict.

Injections are carried out after abortion, miscarriage, surgery to prevent intrauterine pregnancy. Also, anti-Rhesus immunoglobulin is administered to pregnant women at risk at week 28 and 34 again to reduce the likelihood of developing hemolytic disease of the fetus. In addition, injections are prescribed within 2-3 days after birth, which reduces the risk of Rhesus conflict in subsequent pregnancies. Immunoglobulin is administered during each pregnancy if it is likely that a child with a positive Rh factor is born.
Thus, the Rh conflict of the mother and the fetus is not a reason for abortion. The likelihood of developing a Rhesus conflict is extremely small, so there is no reason to despair. Thanks to the modern achievements of immunology, there is always the opportunity to endure a strong and healthy baby.