Streptoderma in children is a fairly common disease that develops against a background of reduced immunity. The causative agents are various strains of streptococcus. The symptomatology of the disease is pronounced, bubble rashes sometimes appear on the mucous membranes, more often on the skin. If treatment is not started in time, then streptococcus affects more and more new areas of the skin.
The incubation period of streptoderma lasts a week, after which the disease begins to develop more actively and develops into an acute form. To avoid complications, after making a diagnosis, it is necessary to urgently begin treatment. The course of the disease can be different: chronic, acute, deep or superficial. In the chronic form, streptococcus is immediately determined when any wounds and sores appear on the skin.
Streptoderma infection
Streptoderma in children is a contagious disease. Most often, it affects young children (2-7 years). The provoking factors that contribute to infection with streptococcus are abrasions, cuts, insect bites, scratches and other damage to the skin. Through them, the infection easily enters the body. How does streptoderma begin in children? An infection can be transmitted through toys, dishes, objects that the sick kid touched, that is, by any household means. Once in a healthy body, after a few days, the infection begins to appear in the form of rashes.
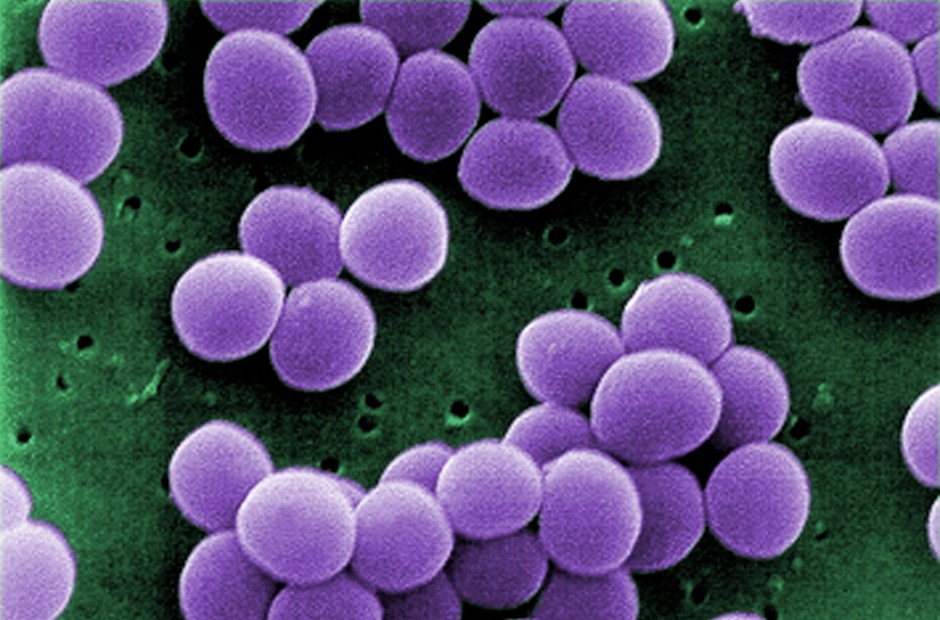
What is streptoderma? The causative agent, as already mentioned, is a streptococcal bacterium (most often group A is predominantly beta-hemolytic pyogenic streptococcus). Its reproduction on the skin leads to the formation of vulgar eczema, impetigo, and some other ailments, which are united by one general concept of streptoderma. You can detect streptococcus not only on toys and dishes, but also on the clothes of the child (both lower and upper), linen must be ironed with a hot iron.
The carrier can be any person (both small and adult), suffering from otitis media, tonsillitis or erysipelas.
Causes of the disease
Streptococcus is a typical representative of the microbial opportunistic flora. If the immune system functions normally, there are no injuries on the mucous membrane and skin, the development of this microorganism becomes limited, streptoderma in children does not develop. In small quantities, certain varieties of these microorganisms are present in the human body, but healthy immunity copes with them.
The inflammatory process begins as soon as conditions favorable for microbes in a fragile body occur, so streptoderma develops in children. The photo shows that there are too many painful vesicles. A sick person becomes dangerous and contagious.
For this reason, often children get sick in children's groups, where they use common household items, toys.
The causative agent is actively spreading with dust, so it is recommended for prophylaxis that wet cleaning is more common. In addition to the listed causes of infection, it is worth adding stress and malnutrition.
In addition to the primary, there is a secondary form of streptoderma. Its causes are diseases that led to violations of the skin. It can be scabies, lichen or eczema. The main reasons for which streptoderma occurs, doctors include the following:
- failure to fully comply with personal hygiene;
- damage to the mucous membrane and skin (cracks, abrasions, seizures, combing of insect bites, etc.);
- stressful situation;
- deterioration of the immune system;
- chronic skin diseases (pediculosis, dermatitis, psoriasis);
- endocrine disorders (diabetes mellitus);
- lack of vitamins in the body;
- with too frequent water procedures, a film having protective properties is washed off the skin;
- with too rare water procedures, dead cells of the dermis and opportunistic microorganisms are not removed;
- frostbite and burns;
- intoxication;
- varicose veins (circulatory disorders).
Streptoderma in children: symptoms and photos
The incubation period of the disease lasts for seven days. The clinical picture of streptoderma in children begins to appear after this period.
Dermatologists divide symptoms into two groups - these are the main and additional. The main ones are those that characterize streptoderma. Additional may occur in other childhood diseases.
The main symptoms of streptoderma in children:
- Redness appears in various parts of the body. Rashes can be on the face, arms, legs, back, buttocks.
- Bubbles later appear, there is a yellowish liquid inside.
- Within two days, the size of the bubbles increases markedly, after which they burst.
- Erosions form on the skin, which become wet, then dry to yellow crusts.
- Crusts disappear over time.
- After this, white spots remain, which gradually disappear.
- Throughout this cycle, the baby’s skin is unbearably itchy.
When combing, the pathogen spreads more, recovery comes later. Streptoderma in children (symptoms are visible in the photo) brings significant discomfort.
The disease lasts from 3 to 7 days, medical advice should be strictly observed.
Additional symptoms include:
- enlarged lymph nodes;
- temperature rise;
- nausea and vomiting
- weakness, impaired appetite, general malaise, lethargy, sleep disturbance.
Many parents, not knowing exactly the symptoms of streptoderma, confuse this ailment with other skin diseases (pityriasis versicolor, urticaria, atopic dermatitis, eczema, pyoderma). The treatment for each disease can be different, so the diagnosis should be established only by a competent specialist. Streptoderma is very diverse. The first vesicles that appear are called impetigo, in their place weeping sores form.
Types of disease
Streptoderma has several varieties, consider the most common of them.
Impetigo streptococcal is the classic and most common form. How does streptoderma begin in children? The photo shows that red rashes appear on the face. They can also form on the hands and feet, on the hands. This form is the most limited, in this case, the infection does not penetrate deeper than the surface layer of the dermis. Its protective functions are retained, while the local protective functions are activated. Against the background of redness, conflicts are formed (bubbles with a clear liquid). When they appear, severe itching begins. After the liquid becomes cloudy, the vesicles open, crust, dry out. After removing the crusts, pigment spots remain on the skin. In a normal course, the disease lasts up to seven days. With complications, it drags on for up to three weeks.
With bullous impetigo, the location of the rash is the lower and upper limbs (feet and hands), the spots are large. After opening the sores grow and capture healthy areas of the skin.
Streptococcal diaper rash most often occurs in infants and overweight people. It is localized in the skin folds: in the axillary hollows, under the mammary glands, in the inguinal-femoral and intergluteal folds.
In the form of dry streptoderma in children, simple lichen is often formed. It appears as a spot with clear borders of bright pink color. It occurs on the face. When exposed to sunlight, the rash decreases. Previously affected areas during tanning have a color different from the rest of the skin.
Streptococcal seizure is one of the varieties of slit-shaped impetigo. Bubbles form in the corners of the mouth. After they disappear, cracks (erosion) form on the affected areas, they become covered with a yellow crust. Children often peel off this crust, but it forms again.
Streptococcal ecthyma is the most severe form of streptoderma. The infection penetrates into the deeper layers of the dermis. With the course of the disease, scars and ulcerative necrotic lesions form. Often this form affects the legs and arms. It does not occur on the face, since there is a fairly good blood supply to the skin, it allows you to quickly cope with inflammatory processes. If the causative agent of ecthyma enters the bloodstream, a person begins to feel general signs of toxic toxic shock, and overall well-being is significantly worsened.
Diagnostics
To know what measures must be taken in the fight against the disease, the doctor must correctly diagnose. Above, it was examined how streptoderma begins in children. At the first suspicion, parents should immediately contact a pediatrician.
The diagnosis is established on the basis of data (an outbreak of streptoderma in a children's team, single contact with an infection carrier) and after a visual examination (multiple vesicles or honey-crusts).
For a more accurate study, laboratory methods are used:
- A smear is taken from the affected area of the skin for microscopy.
- A part of the crust is sown on a nutrient medium (bacteriological analysis).
These methods are used before taking antibiotics and in the event that no self-medication has been used.
When making a diagnosis, a competent doctor relies on all the data:
- Clinical signs. The external manifestations of an infectious disease are taken into account, the nature of its appearance is established.
- Bacteriological methods. Scraping is taken from the skin for inoculation, the contents of the vesicles are examined, as well as purulent discharge with erosive damage to the dermis.
- The sensitivity of the child to various antibiotics when prescribing therapy is taken into account.
- Additional examination methods include: egg test, biochemical and general blood tests, urinalysis. The results make it possible to judge how the inflammatory process in the body develops, which course of treatment should be chosen.
- Differential diagnosis. Any pediatrician knows that streptoderma can mask other diseases with similar symptoms. These are fungal infections, staphylococcal pyoderma, syphilis, herpes, chickenpox. Only after collecting all the data, the doctor establishes the correct diagnosis and prescribes treatment.
Streptoderma treatment
Treatment of streptoderma (on the face of a child or in other parts of the body) must be carried out correctly, adhering to all the doctor's recommendations.
There is a whole range of therapeutic measures that will help to cope with the disease. One of them is the use of antibacterial drugs. These drugs are used both externally and internally. Doctors do not prescribe such an aggressive form of treatment if the manifestations of streptoderma are single or mild. If parents know how streptoderma begins in children (photo is presented), then their timely treatment will help to avoid an acute form of the disease. The doctor prescribes antibiotics only in those cases when the process is actively developing and it is difficult to stop it. In exceptional cases, the use of hormonal drugs may even be required.
Topical antibiotic ointments:
- erythromycin;
- tetracycline "
- Linkomycin;
- Gentamicin;
- Mupiracin;
- Bactroban
- "Baneocin";
- Levomikol;
- “Syntomycin”;
- "Altargo";
Hormonal ointments used in rare cases:
- "Belogent";
- Lorinden S;
- Canizon Plus;
- Betaderm;
- Triderm.
With systemic treatment, doctors prescribe antibiotics of the penicillin group, macrolides, cephalosporins. Penicillins are not prescribed in cases where the child has recently received such an antibiotic in the recent past for any other disease, or if his history shows hypersensitivity or intolerance to this group of drugs.
Local treatment
What medications are used, it became clear, and how to treat streptoderma in children (the first symptoms are visible in the photo) before going to the doctor, when the baby begins to act up and comb sore spots.
Funds that are in any home medicine cabinet come to the rescue:
- hydrogen peroxide;
- salicylic alcohol;
- boric acid;
- fucorcin;
- zelenka.
Antiseptics must be applied correctly, with knowledge of the matter. The vial is opened very carefully, then with a cotton swab, the product is applied to the affected area with a grip around the site by 1-2 mm. The antiseptic should dry completely.
What streptoderma looks like in children should be known to all parents and take timely measures to alleviate the condition of the child.
The use of decoctions of medicinal plants is recognized even by official medicine. Helps relieve itching and inflammation of lotions from a string, calendula, chamomile, oak bark.
But all these funds are used only as auxiliary, in combination with drug therapy.
Streptoderma in children: treatment at home
Below are recipes that have been used for many years in traditional medicine. For skin diseases, these remedies help alleviate the course of the disease.
A photo of streptoderma in a child's face indicates redness, rashes, which bring an unbearable sensation to the baby. Using decoctions, you can remove unpleasant symptoms.
- Decoction of oak bark decoction is famous for its anti-inflammatory properties. Take 0.5 liters of water and pour a tablespoon of dry raw materials. Boil for half an hour. Cool and strain the broth. It is better to treat affected areas of the skin early in the morning and at night.
- For lotions, a decoction from a string or calendula is used. 300 ml of water is taken for 20 grams of raw material, everything is put in a glass dish and aged in a water bath for 40 minutes. In a warm form, it is applied to the affected areas (you can use cotton pads, pads).
- Sage broth helps a lot. Pour 0.5 liters of water into a half glass of chopped grass and boil for ten minutes. Strain the broth and take it inside. Give the child 50-100 ml between main meals. For lotions, you can use a cake from straining, pre-wrapping it in a cloth.
Personal hygiene
We examined streptoderma in children, photos and treatment were also presented. And what needs to be done so that the disease goes away as quickly as possible and does not appear at all in the future? Pay attention to the personal hygiene of the baby. Remember:
- The first 3-4 days, you should not bathe the baby, water quickly conducts the infection on the unaffected areas of the skin.
- Wipe areas of the skin that are not captured by the infection, daily wipe with a cotton swab moistened with decoctions of herbs.
- Make sure that the baby does not comb the sores. With intolerable itching, the doctor may prescribe suitable antihistamines.
- Allocate separate household means to the child: dishes, a towel. After using them, immediately carry out a thorough treatment.
- Remove all soft toys for the duration of the illness. Plastic are washed daily in boiled water and treated with antiseptics.
- Bed sheets need to be changed daily, ironed with a hot iron, especially pillowcases.
- Any skin lesions must be treated with antiseptic solutions.
By following all these measures, you can help your child. The disease will pass in a mild form and in an extremely short time. Otherwise, if the infection spreads to healthy areas of the skin, the disease may worsen and drag on for a long time.
Prevention
In order to prevent further relapse of streptoderma in a child on the face or other parts of the body, strictly monitor the health of your baby. Provide him a balanced diet, monitor hygiene. To increase immunity, walk more often, sign up for a pool, and use vitamin complexes. In case of any damage to the skin, immediately disinfect the wounds, this will close the entrance for the penetration of various infections.
Remember the main points for the prevention of any infectious diseases. Their implementation will allow your child to learn from childhood to protect his body from many diseases:
- Strictly observe the rules of personal hygiene.
- A healthy child should wash daily and take a bath or shower.
- Every day you need to change underwear.
- Inflammatory skin lesions must be properly and promptly treated.
- A healthy lifestyle is important.
- Spend more time outdoors, in nature.
- Be sure to do sports.
- Temper your child from birth.
- Provide your baby with a complete and balanced diet.
As you can see, ensuring a baby a healthy life is not at all difficult. All loving parents, with strict adherence to our recommendations, will be able to avoid infectious diseases in the child, and when they appear, cope with them in a short time.